- To take down chance of contracting COVID-19, public health professionals recommend remaining 6 ft from people outdoors your “bubble,” but professionals state that isn’t always enough.
- The 6-feet rule goes back towards the late 1800s, whenever a German researcher discovered that pathogens were contained in large tiny droplets expelled in the mouth and nose.
- However, wind and weather can impact how tiny droplets travel. When the humidity is low, bigger tiny droplets can shrink and remain in mid-air longer.
Anywhere you go in public places nowadays, signs, barricades, and stickers help remind you to definitely remain at least 6 ft from others to be able to lessen the spread from the coronavirus that triggers COVID-19.
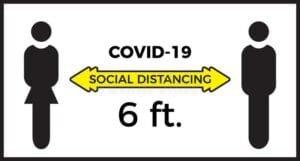
This really is physical distancing, also referred to as social distancing, and it is a vital public health tool for ending the COVID-19 pandemic.
Regrettably, states Lydia Bourouiba, PhD, director from the Fluid Dynamics of Disease Transmission Laboratory at Durch, the 6-feet rule is dependant on outdated science.
She and her colleagues write inside a new paper printed Tuesday within the medical journal BMJTrusted Source there are many situations where 6 ft isn’t enough to maintain your risk low.
Origin from the 6-feet rule
The 6-feet rule goes back towards the late 1800s, when German researcher Carl Flügge discovered that pathogens were contained in large tiny droplets expelled in the mouth and nose. Many of these tiny droplets fell down within three to six ft of the individual by having an infection.
Within the 1940s, advances in photography enabled researchers to capture pictures of these expiratory tiny droplets being sprayed whenever a person sneezed, coughed, or spoken.
Other studies around that point discovered that large particles rapidly fell down close to the person expelling them, reinforcing the 6-feet rule – regardless of limitations from the precision of those early studies.
These studies tended to group expiratory tiny droplets into two groups: small and big. Scientists thought large tiny droplets would fall rapidly down and small tiny droplets would evaporate before they were given far, unless of course pressed by another air flow.
However, “in the final 90 years, we’ve many userful stuff here much more about what’s really happening … whenever you speak or cough or sneeze,” stated Jesse Capecelatro, PhD, a helper professor of mechanical engineering in the College of Michigan in Ann Arbor, who wasn’t active in the new study.
He states many factors can impact what lengths tiny droplets are dispersed. When the humidity is low, bigger tiny droplets can shrink and remain in mid-air longer. Wind outdoors or ventilation inside may also carry tiny droplets farther away.
“This whole concept that there’s this 6-feet perimeter, and when you’re 1 inch beyond after that it you’re safe, really doesn’t make much sense,” stated Capecelatro.
Inside a recent systematic review, 8 of 10 studies reviewed discovered that expiratory tiny droplets could travel greater than 6 ft from individuals with infections, and perhaps as much as 26 ft.
Research using the coronavirus that triggers COVID-19 supports the concept that 6 ft might not continually be enough. In a single study, researchers found the transmission distance from the virus may depend on 13 ft. In another, they detected it on multiple air ventsTrusted Source inside a patient’s room.
There’s even the situation from the choir practiceTrusted Source in Washington condition in March, where one individual with COVID-19 signs and symptoms transmitted herpes to a minimum of 32 other singers. The forcefulness from the exhalation while singing is believed to possess helped herpes spread, but additional factors for example discussing snacks might have been involved.
Air flow patterns affect droplet travel
Among the key messages of physical distancing is when you’re outdoors, your chance of contracting the coronavirus is usually less than if you are inside. It is because herpes is much more rapidly diluted – meaning you’re uncovered to less particles.
“If you’re inside a room and someone coughs, sneezes, or speaks, the tiny droplets they expel can hold off for any lengthy time,” stated Capecelatro. “It makes no difference where you stand within the room. You will be inhaling a number of individuals tiny droplets, particularly if there’s poor ventilation.”
A preprint paper by Japanese researchers discovered that the chance of transmission inside is eighteen.7 occasions greater compared to outside risk. This paper is not peer-reviewed, therefore the results ought to be viewed with a few caution.
However, not every indoor settings are produced equal. Air flow patterns matter and often can worsen.
“What the air flow can perform, particularly if it’s turbulent, is cause these [virus] particles to cluster, which will increase the amount of particles you could inhale,” stated Capecelatro.
He and the colleagues lately simulated how virus particles exhaled by passengers would spread all through a bus, to be able to prevent people riding the College of Michigan buses.
Some studies support the concept that poorly ventilated spaces are riskier.
In a single situation in China, 10 individuals from three families who visited a cafe or restaurant contracted the coronavirus over one hour. Not one of them had direct physical connection with the individual using the virus – some were sitting upright to fifteen ft away.
Outbreaks are also reported at other indoor settings, including gyms, sales departments, and places of worship.
Numerous studies, though, only have checked out average air flow rates, not fluctuations within the movement of air inside a space.
Another preprint study on researchers in the College of Minnesota College of Science and Engineering looked in greater detail at just how the coronavirus spreads inside when exhaled by individuals. They examined three specific settings – a lift, a little classroom, along with a supermarket.
They discovered that good ventilation can remove a few of the virus particles in the air, however, many will finish on surfaces within the room.
Study author Jiarong Hong, PhD, an affiliate professor of mechanical engineering in the College of Minnesota, stated if individuals surfaces aren’t cleaned frequently, people may get the particles once they touch the surfaces. The particles may also be resuspended in mid-air and inhaled.
In some instances, poor ventilation may cause “hot spots,” places where herpes particles congregate. Hong’s studies have shown how you can fix a few of these problems.
“Our tools can predict the existence of locations [inside a setting] and the way to potentially alter the ventilation system in individuals spaces to reduce risks,” stated Hong.
Although each space is exclusive and needs another method of lowering the spread of coronavirus, Hong stated there are several general approaches that companies may take to improving their spaces.
Including putting ventilation sources close to the major virus emitters – for example in which a teacher stands inside a classroom – to be able to capture as most of the particles as you possibly can. Opening home windows is yet another option that many spaces can usually benefit from, he states.
Hong’s research around the spread of coronavirus within different settings offers some insights into how people can help to eliminate their risk in various settings.
“When one enters an area, you are able to assess the potential [coronavirus] risk,” he stated, searching at items like how crowded the area is, whether individuals are putting on masks and also the air flow.
“For example, if you need to get into a little space that’s poorly ventilated, you are able to decide whether you need to use there or if you wish to shorten your time and effort for the reason that space. They are both steps you can take to take down risk.”